
The oculovestibular responses and oculocardiac are less frequently tested, except to determine brain death. Pupillary light, corneal, oculocephalic, and gag reflexes are routinely assessed in the critical care setting. Assessment of pupillary size allows the diagnosis of third nerve lesion (i.e., mydriasis) or Horner’s syndrome (i.e., myosis, ptosis, enophtalmia, and anhidrosis). Abnormal spontaneous eye position and movements may be encountered in patients with brainstem lesions and can be seen in comatose patients. The testing of the cranial nerves and brainstem reflexes is described in Table 3. A brainstem lesion of the posterior column-medial lemniscus pathway and the spinothalamic tract results in a contralateral proprioceptive/touch and temperature/pain deficit, respectively. Bilateral motor corticobulbar tract lesion may present with swallowing impairment, dysphagia, dysphonia, velo-pharyngo-laryngeal impairments, uncontrollable crying/laughing episodes, and emotional lability (i.e., pseudobulbar affect Table 2). Brainstem lesions may present with abnormal movements, such as hemichorea, hemiballism, dystonia, tremor, asterixis, pseudo-athetosis, and non-epileptic myoclonus (Table 2). Characteristic clinical features of brainstem lesions include ipsilateral cranial nerve palsies or cerebellar signs combined with contralateral motor deficits. It usually results from bilateral pontine white matter lesions. Upper motor neuron damage can lead to symptoms, ranging from hemiparesis to the locked-in syndrome, which is typically characterized by intact awareness, quadriplegia, anarthria, and absence of eye movements except for preserved vertical gaze.

While the former controls voluntary movement, the latter is involved in reflexes, motion, complex movements, and postural control (Tables 1 and 2). The pyramidal and extrapyramidal tracts connect the upper motor neurons and the extrapyramidal nuclei with the lower motor neurons located in either the brainstem or the spinal cord. Brainstem motor and sensory deficits and cranial nerve palsy In the present review, we describe brainstem functional neuroanatomy, clinical syndromes, and assessment methods before addressing the concept of critical illness-associated brainstem dysfunction.īrainstem pathology should be considered in cases of (a) sensory or motor deficits combined with cranial nerve palsy, (b) impairment of consciousness, (c) dysautonomia, or (d) neurological respiratory failure.
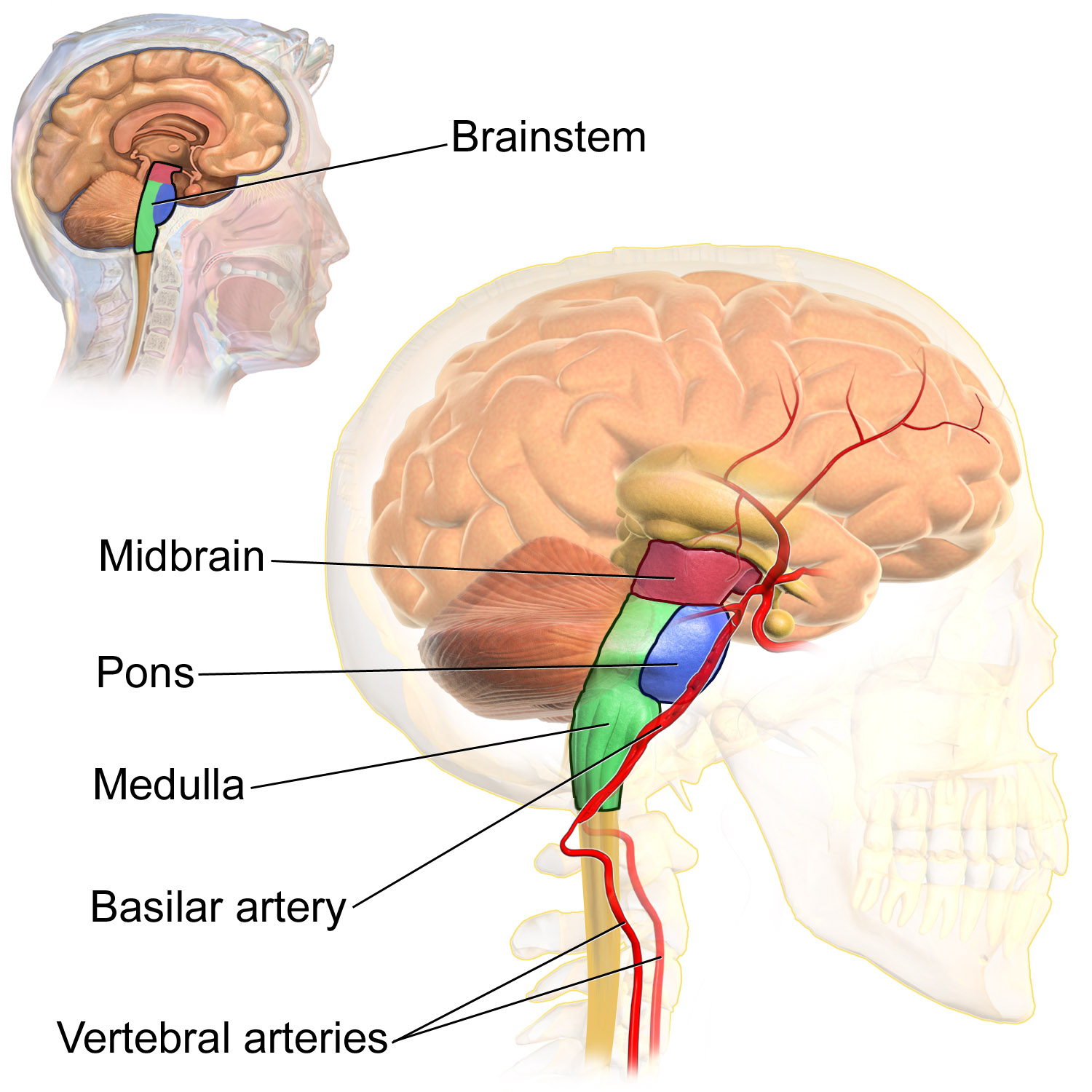
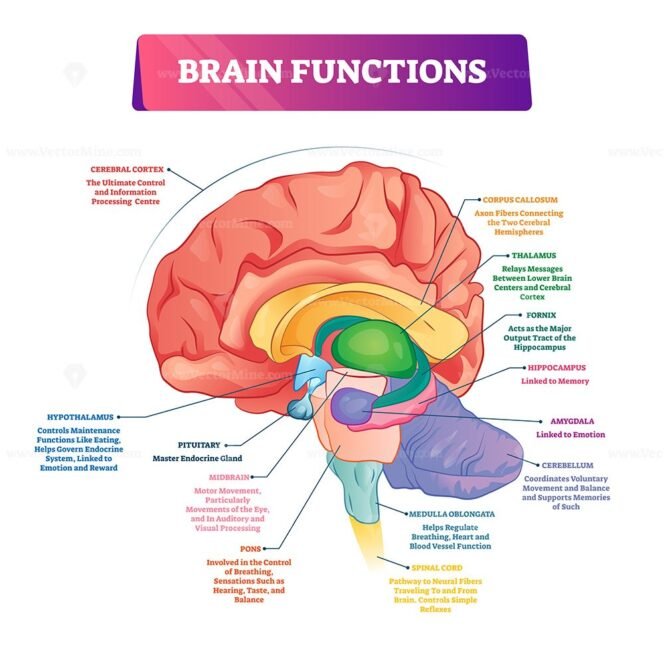
Brainstem dysfunction can then contribute to impairment of consciousness, cardiocirculatory and respiratory failure, and thus increased mortality. In the context of critical illness, the brainstem can be susceptible to various insults that can be categorized as structural and non-structural origin. Brainstem dysfunction may result from various acute or chronic insults, including stroke, infectious, tumors, inflammatory, and neurodegenerative diseases. It controls the brainstem reflexes and the sleep-wake cycle and is responsible for the autonomic control of the cardiocirculatory, respiratory, digestive, and immune systems. The brainstem mediates sensory and motor pathways between the spinal cord and the brain and contains nuclei of the cranial nerves, the ascending reticular activating system (ARAS), and the autonomic nuclei. The brainstem is the caudal portion of the brain that connects the diencephalon to the spinal cord and the cerebellum. In the present review, we summarize the neuroanatomy, clinical syndromes, and diagnostic techniques of critical illness-associated brainstem dysfunction for the critical care setting.
Detection of brainstem dysfunction is challenging but of utmost importance in comatose and deeply sedated patients both to guide therapy and to support outcome prediction. Of particular importance for characterizing brainstem dysfunction and identifying the underlying etiology are a detailed clinical examination, MRI, neurophysiologic tests such as brainstem auditory evoked potentials, and an analysis of the cerebrospinal fluid. The brainstem is prone to various primary and secondary insults, resulting in acute or chronic dysfunction. Brainstem dysfunction may lead to sensory and motor deficits, cranial nerve palsies, impairment of consciousness, dysautonomia, and respiratory failure. It controls the sleep-wake cycle and vital functions via the ascending reticular activating system and the autonomic nuclei, respectively. The brainstem conveys sensory and motor inputs between the spinal cord and the brain, and contains nuclei of the cranial nerves.


 0 kommentar(er)
0 kommentar(er)
